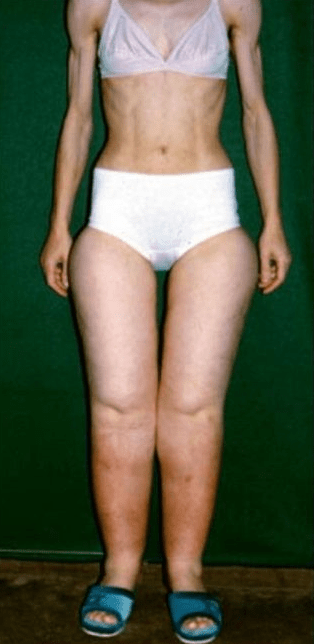
If you’ve ever wondered why your legs seem disproportionately large compared to the rest of your body—or why dieting and exercise don’t seem to shrink stubborn fat in your lower half—you might be looking at something more than just weight gain or cellulite. Lipedema is a chronic fat disorder that affects millions of women, but it often goes undiagnosed or is mistaken for obesity. While only a trained specialist can make an official diagnosis, this article will walk you through key symptoms and self-checks to help you with self-diagnosis and better advocate for yourself.
What Is Lipedema?
Lipedema (pronounced LIP-uh-dee-muh) is a disorder of fat distribution that primarily affects women. It causes the abnormal accumulation of painful fat, usually in the legs, hips, buttocks, and sometimes arms—sparing the hands and feet. This condition is progressive and resistant to traditional weight loss methods.
The Most Common Signs and Symptoms
Here’s what to look for when doing a self-diagnosis check:
- Disproportionate lower body fat: Fat often builds up symmetrically on both legs or arms, even if your upper body remains lean.
- Column-like or “tree trunk” legs: The legs may appear thick and uniform in size from thighs to ankles, often ending abruptly at the ankles or wrists.
- Cuffing at the ankles or wrists: There’s usually a sharp demarcation where fat ends and normal tissue begins.
- Tenderness or easy bruising: The affected areas are often painful to the touch and bruise more easily than normal.
- Swelling that worsens throughout the day: While fat is the primary issue, swelling (especially from standing or heat) is common and may reduce overnight.
- Negative Stemmer’s Sign: You can pinch the skin at the base of the toes or fingers—if you can lift the skin, that’s a negative result and points toward lipedema rather than lymphedema.
The “Float Test” – Lipedema Fat Is Buoyant
One interesting self-test is to check for buoyancy. Women with lipedema often find that their legs float more easily in water. This is because lipedema fat has a higher fluid and connective tissue content. Try relaxing in a bathtub or pool and notice if your legs tend to float more than expected.
Palpation Test: Check the Cubital Area
Another helpful self-check is palpation of the cubital area, which is the inside crease of your elbow. Gently press this area with your fingers. Women with lipedema may feel small nodules, lumps, or even discomfort. Similar nodules might be found in the thighs or upper arms.
Understanding the Stages of Lipedema
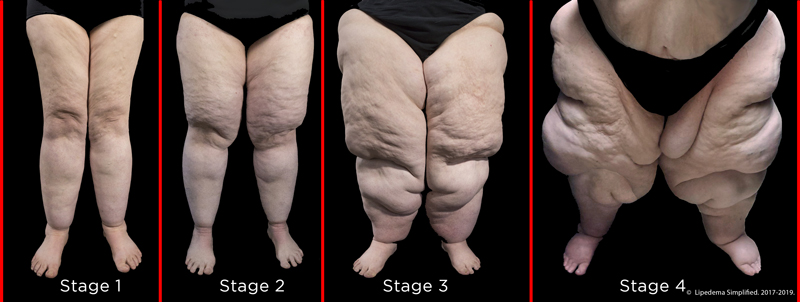
Lipedema progresses through four distinct stages:
- Stage 1: Smooth skin surface with soft, evenly distributed fat. Swelling comes and goes.
- Stage 2: Uneven skin with indentations or “mattress-like” texture. Fat becomes harder and more nodular.
- Stage 3: Large fat lobes form, particularly around the knees or thighs. Mobility may start to decline.
- Stage 4 (Lipo-lymphedema): Advanced fat accumulation with concurrent lymphedema. This stage includes significant swelling, hardening of tissue, and more functional limitations.
When Does Lipedema Get Worse?
Lipedema tends to worsen during times of hormonal change, including:
- Puberty
- Pregnancy
- Perimenopause and menopause
- Starting or stopping hormonal birth control
If you noticed sudden changes in your body shape during these times, particularly in your lower half, it might be worth looking into.
How to Tell Lipedema Apart from Cellulite or Obesity
While cellulite and general weight gain affect many women, lipedema is distinct in these ways:
| Feature | Lipedema | Cellulite | Obesity |
|---|---|---|---|
| Symmetrical fat accumulation | ✅ | ❌ | Sometimes |
| Pain or tenderness | ✅ | ❌ | Sometimes |
| Swelling throughout day | ✅ | ❌ | Sometimes |
| Hands/feet unaffected | ✅ | ✅ | ❌ |
| Bruising easily | ✅ | ❌ | ❌ |
| Responds to diet/exercise | ❌ | ✅ | ✅ |
What to Do If You Suspect Lipedema
If you’ve done a self-diagnosis and recognize these symptoms, the next step is to seek out a specialist, preferably one familiar with lymphatic disorders or who has experience diagnosing and treating lipedema. Many general practitioners are unfamiliar with this condition and may misdiagnose it as simple obesity.
You might want to bring documentation, pictures of your body changes over time, and a symptom diary to your appointment to help make your case.
Final Thoughts
Learning about lipedema can be both enlightening and emotional—especially if you’ve struggled with body image, dieting, or unexplained pain for years. While a formal diagnosis is essential, becoming educated and self-aware can be the first empowering step toward healing and advocacy.
If you suspect you might have lipedema, you’re not alone. Keep learning, seek out community, and most importantly, don’t give up on finding answers.